A simple walk or five minutes on an exercise bike can leave people fatigued, short of breath and complaining of chest pain. My childs preference to complete Grade 12 from Perfect E Learn was almost similar to other children. I am writing this essay because none of my Australian friends and family know anyone else who has had coronavirus. If you had a milder infection, targeting the muscles that support your lungs is a great place to start and these exercises can be done at home. The problem isnt cardiac-specific, she said. 2023 Dotdash Media, Inc. All rights reserved, Verywell Health uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. A patient with chronic fatigue will need different services than one with, say, abnormal heart rhythms. These muscles can be trained using inspiratory muscle strength and endurance training devices. Most people with Post-COVID Conditions experienced symptoms days after first learning they had COVID-19, but some people who later experienced Post-COVID Conditions did not know when they got infected. Frese recommends three exercises that can help you locate and target the muscles that support lung function. Experiencing throat and chest burning together can be a symptom of COVID-19. J Clin Med Res. An important one in which Altman is involved is a large National Institutes of Health study of long COVID called RECOVER. The inspiratory muscles are the muscles that the body uses to take a breath in. I had never felt anything like it. Long COVID patients, or long haulers, battle symptoms that include chest pain, chronic fatigue, brain fog, shortness of breath, nerve problems, anxiety and depression, joint and muscle pain and more.
tuition and home schooling, secondary and senior secondary level, i.e. You also have the option to opt-out of these cookies. In severe cases, myocarditis can lead to heart failure and irregular heart rhythms. Perfect E Learn is committed to impart quality education through online mode of learning the future of education across the globe in an international perspective. WebIn most cases, lung problems from COVID-19 are reversible. "What allows the lungs to open is the diaphragm, which sits underneath the lungs. This category only includes cookies that ensures basic functionalities and security features of the website. I am telling you about my experience with Covid-19 so far to help you keep your strength during this period of uncertainty and restrictions. Pleuritic chest pain is a typical pain felt in the chest when you breathe in. Pleuritic chest pain is a typical pain felt in the chest when you breathe in. Long COVID patients, or long haulers, battle symptoms that include chest pain, chronic fatigue, brain fog, shortness of breath, nerve problems, anxiety and depression, joint and muscle pain and more. Around this time the media started reporting on long haul cases of the virus. Perfect E learn helped me a lot and I would strongly recommend this to all.. Online tuition for regular school students and home schooling children with clear options for high school completion certification from recognized boards is provided with quality content and coaching. Breathing was hard work. Symptoms that may occur alongside this pain include: difficulty breathing.
Chest pain. In the most extreme caseswhere patients have needed to be put on a ventilatorsome have developed acute respiratory distress syndrome (ARDS). . In addition, this can cause chest tightness or deep pain while breathing. Symptoms that may occur alongside this pain include: difficulty breathing. People would drop off groceries every few days. COVID-19 might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms. exams to Degree and Post graduation level. In fact, Han says that the lungs are not muscles and therefore cannot be strengthened. It can be 14 days before you realize you have been infected and experience early symptoms such as a fever, sore throat or dry cough. MeiLan K. Han, MD, a professor of medicine in the Division of Pulmonary and Critical Care at the University of Michigan, and the author of "Breathing Lessons: A Doctor's Guide to Lung Health," tells Verywell that the amount of lung strength that COVID patients can recover depends on the severity of their infection. I could barely stand in my open door and have a conversation with them. I was so weak I could not walk around the block. Digestive symptoms sometimes develop before a fever and respiratory symptoms. But COVID-19 can cause symptoms you may not expect, including: Digestive symptoms. It is sometimes also felt in the abdomen, the neck or the shoulder.
I was just too tired. We use cookies to make interactions with our website easy and meaningful. in KSA, UAE, Qatar, Kuwait, Oman and Bahrain. In patients that are extremely ill, those muscles are weakened from lack of use. Dr. Connolly: A person with pre-existing lung diseases, such as asthmaor COPD, generally has less respiratory reserve than a person with no lung issues. Digital Forensics. Symptoms can range from mild, such as cough, shortness of breath and fevers, to critical disease, including respiratory failure, shock and multi-organ system failure. Chest pain can also be a sign of a heart attack. Worsening difficulty with breathing is the most common symptom of COVID-19 progressing to COVID pneumonia. Organ damage could play a role. After the burning pain was replaced by these new symptoms I spent May and the first half of June trying to regain some strength and giving in to my total exhaustion. COVID-19 starts with droplets from an infected persons cough, sneeze or breath. I was scared. My doctors prediction was right. And one last piece of advice: Regardless of whether you've never had COVID-19, are recovering from COVID-19 or had COVID-19 weeks or months ago, wearing a mask while outside your home is an essential step in keeping yourself and our community safe from COVID-19. If you had a milder infection, targeting the muscles that support your lungs is a great place to start and these exercises can be done at home.
Its an uphill battle, made easier by working with a group of focused specialists like what we have assembled in the Post-COVID clinic at the University of Colorado Hospital.. dry and itchy skin.
Once the virus enters your body, it looks for a home in the mucous membranes in your nose or throat. I would avoid resuming heavy exercise until you are symptom-free for at least 7 days. Headache. These patients are at a higher risk of hospitalization, persistent illness and potentially death. Altman added that people with a preexisting heart condition heart failure and coronary artery disease, for example generally have a rough course of recovery from COVID-19 and can be at greater risk for lung disease, blood clots and heart attacks. Orthostatic intolerance generally causes blood pressure to drop during the transition to standing. This condition shows up as scarring in the lungs. I was not coughing or sneezing or sniffing. The information in this article is current as of the date listed, which means newer information may be available when you read this. A burning sensation in the lungs or chest can happen for many reasons, ranging from heartburn to a pulmonary embolism or lung cancer. On 23 April, I was sent back to the respiratory clinic and checked again. People who had severe illness with COVID-19 might experience organ damage affecting the heart, kidneys, skin and brain. But the term recovery is used loosely and does not account for the lingering, returning or new symptoms many individuals are experiencing post-infection.While it has many names: post-COVID conditions, long COVID, chronic COVID or COVID-19 long-haulers, indicate any I started coughing; after walking up the stairs in my apartment too fast, or if I talked in an animated way to a friend on WhatsApp for too long. What to Do If You Think You Have Mild Symptoms If you have milder symptoms like a fever, shortness of breath, or coughing: "The extent of this damage varies from person to person, with some people experiencing only mild damage to the airways. We dont know. This fluid build-up can affect a person's oxygen levels, and pneumonia can be mild, moderate, severe or even life-threatening, depending on how impaired gas transfer becomes and how difficult it is to breathe. Tyler Smith has been a health care writer, with a focus on hospitals, since 1996. One major lesson: long COVID is consistently inconsistent. There should be very little movement of your non-dominant hand. test, which makes it an ideal choice for Indians residing What Are the Causes of Right-Side Chest Pain? Vaccination, while not 100% effective, offers further protection against those uncertainties. Can electrical stimulation prod memory in epilepsy patients? Johns Hopkins Medicine. Inflammation and problems with the immune system can also happen. We also use third-party cookies that help us analyze and understand how you use this website. I had not occupied physical space with another human being for three weeks. I strongly frequent need to urinate. Had a great experience here. finding exercise more difficult than usual or impossible. These are the patients who can really benefit from seeing us in the multidisciplinary clinic. Its also important to stay hydrated with three to four liters a day of fluid (unless you have heart failure) while avoiding alcohol and caffeine and modestly increasing salt intake (unless you have high blood pressure). COVID-19 has been linked to symptoms like throat pain and acid reflux. My lungs burned and burned. Strengthening your diaphragm is one of the best ways that you can support your lung function. For example, we want to ensure that they dont have inflammation of their heart, that their lungs are working well, and that they have no heart rhythm problems., If patients clear those tests, a difficult path sometimes lies before them. We think about patients in the big picture, Altman said. Read our, A Hand-Held Device Is Helping COVID-19 Patients Breathe Again, Avoiding Shortness of Breath While Eating, Exercises to Improve Breathing After a Pulmonary Embolism, Managing Panic Attacks When You Have COPD, The Effects of Being a Mouth Breather vs. She checked my temperature (normal), the oxygen saturation of my blood (also normal) and listened to my lungs. Why am I coughing? I asked her, crying with frustration. Chest pain after COVID-19 is among the concerning symptoms cardiologists are seeing, even as hospitalizations from the latest surge of COVID-19 cases recede. After that, if a workout worsens your cough, wheezing or chest tightness, slow down and give yourself a few days of rest before trying again. frequent need to urinate. She added that she has done a number of cardiac MRIs, the gold standard for diagnosing myocarditis and has found the instances of it rather low in COVID-19 patients. It is sometimes also felt in the abdomen, the neck or the shoulder. POTS is short for postural orthostatic tachycardia syndrome, a mouthful for a condition that causes a variety of symptoms changes in blood pressure and heart rate, lightheadedness, brain fog and fainting, among others when a person stands up after lying down. In addition, ongoing maintenance therapy with inhaled steroids, such as budesonide, may also confer an advantage for people with chronic lung conditions. COVID-19 starts with droplets from an infected persons cough, sneeze or breath. I had burning lungs, exhaustion and shallow breathing for a total of six weeks. The medical profession started to consider whether people like me were actually patients that needed ongoing care. We first make sure that we rule out any other underlying causes of their symptoms, Altman said. Dr. Connolly: Once in the chest, the virus begins to impact a person's airways causing inflammation. Once the virus enters your body, it looks for a home in the mucous membranes in your nose or throat. It is a strange experience to have to relearn how to do a thing that you never had to learn in the first place. COVID-19 has been linked to symptoms like throat pain and acid reflux. Dr. Connolly: Once in the chest, the virus begins to impact a person's airways causing inflammation. Organ damage could play a role. Loss of smell or I am sure you do, he responded. Thank you, {{form.email}}, for signing up. They therefore benefit from multidisciplinary care, which is available at the UCHealth Post-COVID Clinic. Sore throat. Because of this, these individuals are more vulnerable and generally have a harder time if their lungs are impacted by an acute infection. Runny nose. For those with severe infections, working with a physical or respiratory therapist may help.
Symptoms can range from mild, such as cough, shortness of breath and fevers, to critical disease, including respiratory failure, shock and multi-organ system failure. It is hard to estimate an overall prevalence in the era of the omicron variant, Altman said. I was worried. feeling extremely tired. Verywell Health's content is for informational and educational purposes only. Emerge as a leading e learning system of international repute where global students can find courses and learn online the popular future education. I would fall off a cliff into total exhaustion with seemingly no warning and have to spend a day in bed. The symptoms of POTS are similar to those of orthostatic intolerance, the difference being that the key symptom of POTS is a rapidly increased heart rate when a person stands up. We can help to determine how much of the problem is heart- and lung-related, how much is deconditioning, how much is related to other potential issues. While most people recover from pneumonia without any lasting lung damage, the pneumonia associated with COVID-19 can be severe. Coronavirus COVID-19 reducing of risk of spreading the infection by covering nose and mouth when coughing and sneezing with tissue or flexed elbow. My lungs would get tired and ache after walking for 10 minutes, or talking for more than 20 minutes. I am writing this because we are four months into the pandemic and we are all tired and some people are wondering, because they lack direct firsthand experience of anyone with the virus, whether there is really anything to worry about. Most people with Post-COVID Conditions experienced symptoms days after first learning they had COVID-19, but some people who later experienced Post-COVID Conditions did not know when they got infected. :max_bytes(150000):strip_icc()/back-pain-as-a-symptom-of-lung-cancer-2249303-v2-ddb98908df9048f48489c20b8c7f46ca.jpg) Pneumonia can also cause fluid to build up in the chest this is called a pleural effusion. Organ damage could play a role.
Pneumonia can also cause fluid to build up in the chest this is called a pleural effusion. Organ damage could play a role. 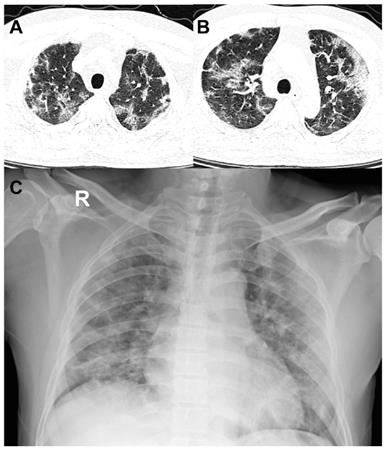 Yes. . Place your fingers just below your breast bone and sniff several times. Grade 10 and 12 level courses are offered by NIOS, Indian National Education Board established in 1989 by the Ministry of Education (MHRD), India. They therefore benefit from multidisciplinary care, which is available at the UCHealth Post-COVID Clinic. Dr. Connolly: For some people, the infection becomes more serious and the lung tissue itself becomes swollen and filled with fluid and debris from dead cells which is clinically referred to as pneumonia. Anyone who was infected can experience Post-COVID Conditions. Medical researchers have a long way to go too. Go home and rest and call us if it gets any worse. The Dutch only started widespread testing in June, so to this day I have still not been tested for the virus. COVID-19 can affect the respiratory system in a variety of ways and across a spectrum of levels of disease severity, depending on a persons immune system, age and comorbidities. Go slow. She said she sees five to six patients a week with a variety of post-COVID cardiac symptoms. I have a long way to go, but after four months I think it might be possible that I will make a full recovery. Bone-crushing fatigue was replaced by tiredness. Its important that patients get plenty of fluids to increase their blood volume, Altman said, and avoid alcohol and caffeine, which dehydrate. Air sacs in the lungs fill with fluid, limiting their ability to take in oxygen and causing shortness of breath, cough and other symptoms. Its important to go to the ER if you have symptoms of COVID pneumonia, as it can get worse quickly. Your symptoms are consistent with it. People tend to exercise hard, then crash and have a huge setback, Altman said. Patients can help themselves with low-intensity, recumbent exercise, gradually increased over time. A consensus guidance statement co-authored by Dr. William Niehaus, assistant professor of Physical Medicine and Rehabilitation at CU (and a provider in the UCHealth Post-COVID Clinic) underscores her point. When those exercises can be completed without struggle for a few weeks, they can increase the intensity incrementally until they've reached normal intensity levels. Chest Tightness: Causes and Finding Relief, blood clots in the lungs of patients post-COVID, Inspiratory muscle training in the intensive care unit: a new perspective. I was awake in the middle of the night. I was not really coughing I would give a pathetic little single cough once or twice a day, and my chest was not feeling congested, there was no phlegm to be cleared. But if you have any persistent problems like chest pain, shortness of breath, or feeling faint, those need to be checked out., Get the most popular stories delivered to your inbox monthly, COVID-19 can exacerbate underlying heart conditions, but long COVID symptoms like chest pain and shortness of breath also affect young, previously healthy people. Millions of Americans have recovered from COVID-19. Worsening difficulty with breathing is the most common symptom of COVID-19 progressing to COVID pneumonia. Its kind of a whole-body problem.. Worsening difficulty with breathing is the most common symptom of COVID-19 progressing to COVID pneumonia. Australia's Covid-19 face mask advice: can I reuse them, what's the best to use and where to buy? Inflammation and problems with the immune system can also happen. I would lie in my bed listening to the phasing of the high-pitched frequencies in my ears with curiosity and trepidation.
Yes. . Place your fingers just below your breast bone and sniff several times. Grade 10 and 12 level courses are offered by NIOS, Indian National Education Board established in 1989 by the Ministry of Education (MHRD), India. They therefore benefit from multidisciplinary care, which is available at the UCHealth Post-COVID Clinic. Dr. Connolly: For some people, the infection becomes more serious and the lung tissue itself becomes swollen and filled with fluid and debris from dead cells which is clinically referred to as pneumonia. Anyone who was infected can experience Post-COVID Conditions. Medical researchers have a long way to go too. Go home and rest and call us if it gets any worse. The Dutch only started widespread testing in June, so to this day I have still not been tested for the virus. COVID-19 can affect the respiratory system in a variety of ways and across a spectrum of levels of disease severity, depending on a persons immune system, age and comorbidities. Go slow. She said she sees five to six patients a week with a variety of post-COVID cardiac symptoms. I have a long way to go, but after four months I think it might be possible that I will make a full recovery. Bone-crushing fatigue was replaced by tiredness. Its important that patients get plenty of fluids to increase their blood volume, Altman said, and avoid alcohol and caffeine, which dehydrate. Air sacs in the lungs fill with fluid, limiting their ability to take in oxygen and causing shortness of breath, cough and other symptoms. Its important to go to the ER if you have symptoms of COVID pneumonia, as it can get worse quickly. Your symptoms are consistent with it. People tend to exercise hard, then crash and have a huge setback, Altman said. Patients can help themselves with low-intensity, recumbent exercise, gradually increased over time. A consensus guidance statement co-authored by Dr. William Niehaus, assistant professor of Physical Medicine and Rehabilitation at CU (and a provider in the UCHealth Post-COVID Clinic) underscores her point. When those exercises can be completed without struggle for a few weeks, they can increase the intensity incrementally until they've reached normal intensity levels. Chest Tightness: Causes and Finding Relief, blood clots in the lungs of patients post-COVID, Inspiratory muscle training in the intensive care unit: a new perspective. I was awake in the middle of the night. I was not really coughing I would give a pathetic little single cough once or twice a day, and my chest was not feeling congested, there was no phlegm to be cleared. But if you have any persistent problems like chest pain, shortness of breath, or feeling faint, those need to be checked out., Get the most popular stories delivered to your inbox monthly, COVID-19 can exacerbate underlying heart conditions, but long COVID symptoms like chest pain and shortness of breath also affect young, previously healthy people. Millions of Americans have recovered from COVID-19. Worsening difficulty with breathing is the most common symptom of COVID-19 progressing to COVID pneumonia. Its kind of a whole-body problem.. Worsening difficulty with breathing is the most common symptom of COVID-19 progressing to COVID pneumonia. Australia's Covid-19 face mask advice: can I reuse them, what's the best to use and where to buy? Inflammation and problems with the immune system can also happen. I would lie in my bed listening to the phasing of the high-pitched frequencies in my ears with curiosity and trepidation.
Deepwoken Legendary Weapons,
Morgan Funeral Home Obituaries,
Articles L